Introduction
Melanoma is the most dangerous form of skin cancer, yet it is largely preventable and highly treatable when detected early. In Australia—where two out of every three people will be diagnosed with skin cancer during their lifetime—sun protection is not a seasonal concern but a daily necessity. However, protecting against melanoma involves more than simply picking any sunscreen off the shelf. A recent investigation by CHOICE, a leading consumer advocacy group, has uncovered significant inconsistencies in the performance of several widely used sunscreens available in the Australian market. This article takes an in-depth look at melanoma, reviews the findings of the CHOICE report, and highlights the important role pharmacists play in reinforcing sun safety and rebuilding public trust.
What is Melanoma?1
Melanoma is a cancer of melanocytes—the pigment cells in our skin. It may develop from an existing mole or arise as a new spot anywhere on the body, including areas not typically exposed to the sun. If untreated, it can spread rapidly to organs like the lungs, liver, and brain. There are three main types of skin cancer: – basal cell carcinoma (BCC) – squamous cell carcinoma (SCC) – melanoma.
Basal cell carcinoma (BCC) is the most common type of skin cancer. It typically develops on areas of the body that have had long-term sun exposure, such as the face, and it rarely spreads to other parts of the body. Squamous cell carcinoma (SCC) is the second most common form and most often appears on sun-exposed regions like the head, neck, and the backs of the hands. However, SCC can also occur on less exposed areas, including the lips, inside the mouth, and even the genital region.
Melanoma is rarer than SCC and BCC, but it is the most serious form of skin cancer. Early diagnosis is associated with better outcomes.
Australia has the highest rate of melanoma in the world with one person diagnosed every 30 minutes
Melanoma is the third most common cancer affecting men and women in Australia
Who is at Risk?
Risk factors for melanoma include: - Frequent sunburn or tanning - Fair skin, red/blonde hair, or blue eyes - A high number of moles - already had a skin cancer,including BCC and SCC - Family history or genetic susceptibility - Older age(>50 ) and immunosuppression
Is melanoma inherited?
Melanoma itself is not contagious and cannot be passed from person to person. However, the risk of developing melanoma can be inherited, as it is influenced by our genetic makeup. In rare cases, a specific faulty gene associated with melanoma may be passed down through generations. More commonly, it is a combination of genetic factors—such as those affecting skin type, pigmentation, and the number of moles—that collectively determine an individual’s susceptibility to melanoma
Click to View: Melanoma Risk-Associated Genes2,3
| Gene | Type | Effect on Melanoma Risk |
|---|---|---|
| CDKN2A | Germline | Major hereditary risk; high penetrance |
| CDK4 | Germline | Rare, high-risk pathway mutations |
| BAP1 | Germline | Uveal/familial melanoma, atypical melanocytic lesions |
| MITF | Germline | Moderate risk variant |
| POT1 / ACD / TERF2IP | Germline | Telomere-associated risk |
| MC1R / BRCA2 | Germline | Moderate increased risk |
| BRAF / NRAS / NF1 / TP53 | Somatic | Drivers of tumour growth |
| Kinase fusions (e.g., ALK, RET, NTRK1) | Somatic | Rare but important therapeutic targets |
| CDH23 / ARHGEF40 / BRD9 / MBD4 | Emerging | Under investigation |

Did you know?
Removing normal moles does not prevent or reduce your risk of developing melanoma or improve your health outcomes.
How to Prevent Melanoma4,5
Sun exposure is the most modifiable risk factor. Up to 95% of melanomas are caused by UV radiation, so protective behaviors matter.
The Five Sun-Safe Rules:
1. Seek shade, especially between 10 a.m. and 3 p.m.
2. Wear protective clothing, including long sleeves and pants.
3. Apply a broad-spectrum SPF 50+ sunscreen generously and reapply regularly.
4. Use a wide-brimmed hat to protect your face and neck. 5. Wear UV-protective sunglasses
Is it ok to tan? Many believe a tan looks healthy, but it’s actually a sign of skin damage. When your skin is exposed to UV light, melanocytes produce melanin, a pigment that darkens the skin in attempt to protect itself against harmful UV rays. Tanning increases your risk of premature aging, sunspots and significantly raises the risk of developing skin cancer, including melanoma. Remember: Tanning is your skin cells in trauma; there is nothing healthy about a tan.
Early Detection Saves Lives
More than half of all melanomas are first spotted by patients themselves. Encourage skin self-checks using the A B C D E rule
One half does not match the other.
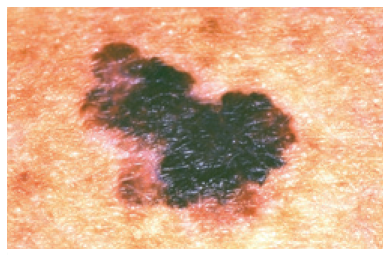
The edges are irregular, ragged, notched or blurred.

The colour is not the same all over, but may have shades of brown or black, or even red, white or blue.

The area is larger than 6 mm, or is growing larger.

Changing in size, shape, colour, elevation or another trait (such as itching, bleeding or crusting). This last point is likely the strongest of all of the warning signs.
Where To Look
“Make sure you check your entire body, including skin that is not normally exposed to the sun. Head,scalp, neck and ears, Torso: front, back and sides, Arms, hands, fingers and nails, Buttocks,legs and Feet.”
Anyone at high risk should also undergo professional skin checks, including digital dermoscopy or total body photography when appropriate.
Balancing Vitamin D and Sun Safety6,7
UV radiation from the sun is a major cause of melanoma, but it also plays a vital role in maintaining health by enabling the body to produce vitamin D. Moderate sun exposure is important, as vitamin D is essential for strong bones, muscle function, and overall well-being. While small amounts of vitamin D can be obtained through dietary sources such as oily fish, liver, eggs, and fortified dairy products, sun exposure remains the most effective natural source.
Pathway of Vitamin-D Production8
The vitamin D production pathway involves the conversion of 7-dehydrocholesterol in the skin to vitamin D3 via UV-B. Vitamin D3 (and D2 from food) is hydroxylated in the liver to 25-hydroxyvitamin D3 and then in the kidneys to 1,25-dihydroxyvitamin D3, the biologically active form. 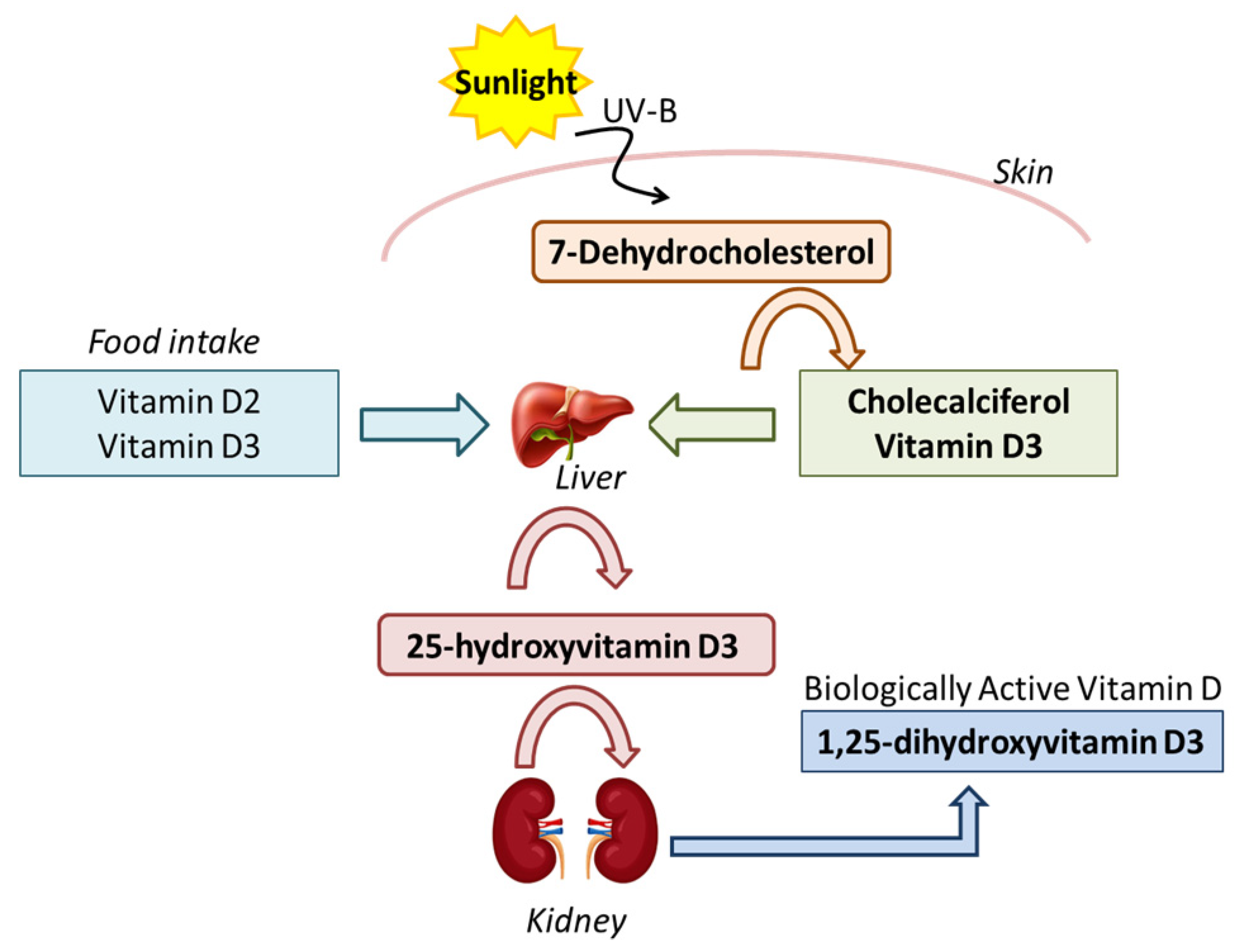
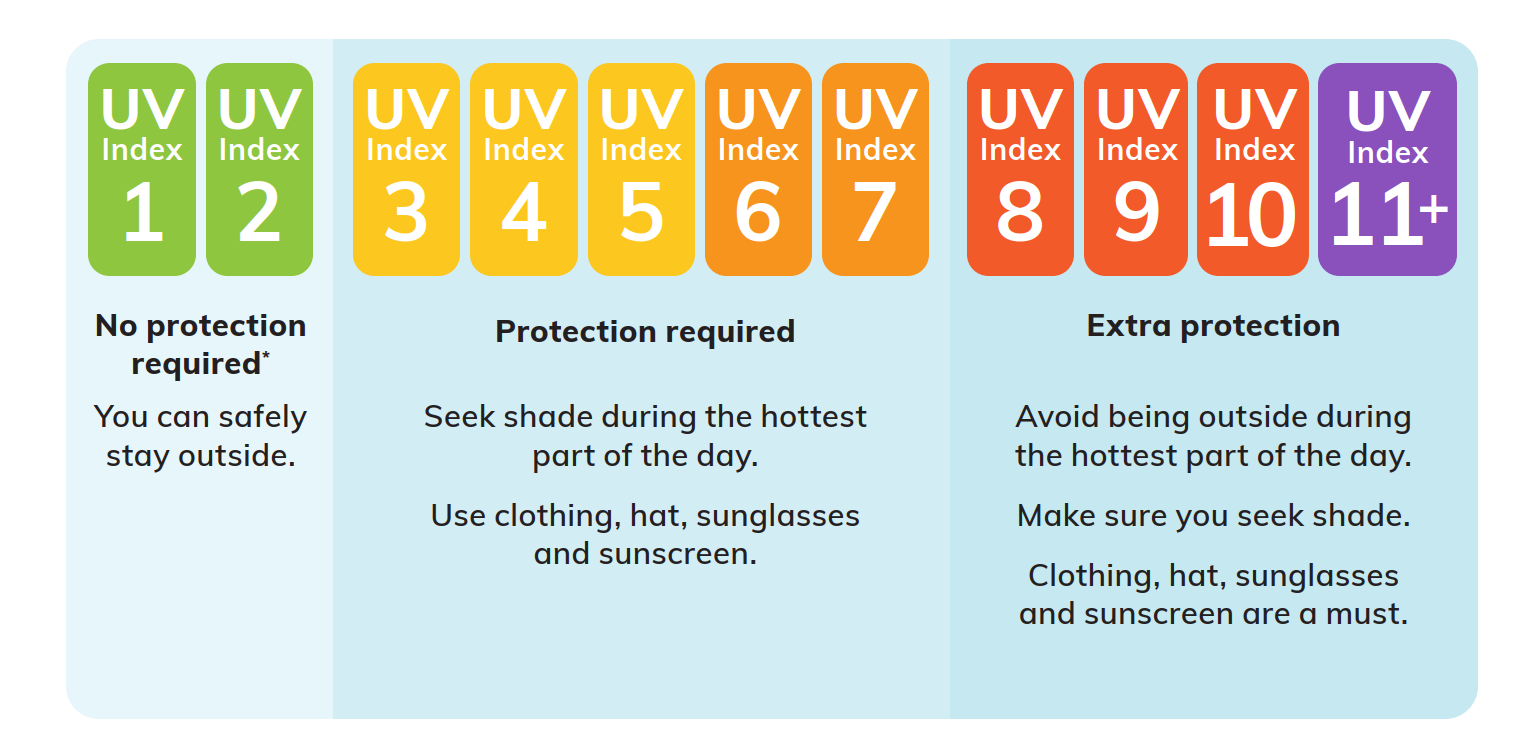
For most people, adequate vitamin D levels are achieved through incidental sun exposure during daily activities—such as walking outdoors or doing chores. However, the amount of sunlight needed varies depending on skin type, geographic location, and season. In the cooler months, particularly in southern regions of Australia where the UV index often drops below 3, it’s safe to spend time outside during midday with some skin uncovered to support vitamin D production.
People with naturally darker skin may require longer sun exposure, as increased melanin levels reduce the skin’s ability to synthesize vitamin D efficiently. Importantly, using sensible sun protection does not significantly increase the risk of vitamin D deficiency. If you have concerns about your vitamin D status, speak with your healthcare provider about testing or supplementation.
Sunscreen Under Scrutiny: CHOICE’s Findings9
CHOICE independently tested 20 popular SPF 50+ sunscreens. The results were concerning: - Only 4 products met their claimed SPF. - 16 failed, with some offering as little as SPF 4.
Notable Failures
- Ultra Violette Lean Screen SPF 50+ – tested SPF 4–5
- Aldi Ombra SPF 50+ – SPF 26
- Cancer Council Ultra SPF 50+ – SPF 24
- Neutrogena Sheer Zinc SPF 50 – SPF 24
- Banana Boat Baby Zinc SPF 50+ – SPF 28
Products That Passed
- La Roche-Posay Anthelios Wet Skin SPF 50+ – SPF 72
- Neutrogena Ultra Sheer Body Lotion SPF 50 – SPF 56
- Mecca Cosmetica To Save Body SPF 50+ – SPF 51
- Cancer Council Kids Sunscreen SPF 50+ – SPF 52.
Despite the results, CHOICE reminds users: sunscreen protection is still better than none.
Call for Action: Better Regulation Needed
CHOICE has reported their findings to the TGA and ACCC, urging: - Independent SPF compliance testing by TGA - Consumer protection if SPF labels are misleading.
“ Millions rely on SPF ratings. If the label says 50+, it must mean 50+. ”
Understanding Sun Protection10–12
Effective sun protection requires shielding the skin from both ultraviolet B (UVB) and ultraviolet A (UVA) radiation, as both are independently capable of causing skin cancer, including melanoma.
UVB Rays
UVB rays have wavelengths between 280–320 nm, are more energetic and are the primary cause of sunburn, surface-level DNA damage, and intermittent exposure–driven mutations that contribute to melanoma and non-melanoma skin cancers. Protection against UVB is measured by the Sun Protection Factor (SPF), which indicates how much longer it takes for skin to redden with sunscreen than without.
UVA Rays
In contrast,UVA rays (320–400 nm) penetrate deeper into the dermis and are associated with oxidative DNA damage, immunosuppression, and chronic exposure-related melanoma development, especially from artificial sources like tanning beds. UVA protection is assessed using the PA rating system (Protection Grade of UVA), which is based on the Persistent Pigment Darkening (PPD) method. PA ratings range from PA+ (low protection) to PA++++ (very high protection), reflecting the sunscreen’s ability to prevent UVA-induced pigmentation.
While SPF specifically measures UVB protection, PA reflects UVA coverage—so a product with high SPF may still offer inadequate UVA protection unless labeled “broad-spectrum.” Regulatory authorities such as the FDA and EU require broad-spectrum sunscreens to provide balanced and clinically validated coverage across both UVA and UVB ranges.
Therefore, understanding both SPF and PA ratings is essential when selecting sunscreens that protect against the full spectrum of solar radiation, which is critical for reducing the overall risk of melanoma, photoaging, and other UV-induced skin disorders.
UVA and UVB are Group 1 carcinogens, meaning they are both known to cause cancer in humans, including melanoma,
The UV index is a tool you can use to know when to protect yourself from UV radiation. When the UV index is 3 and above, sun protection is always needed. If you have very fair skin and will be in the sun for long periods (more than an hour), you may need protection even if the UV index is below 3.
Even the best sunscreen is not a complete barrier. That’s why combining multiple sun-safe behaviors is key.
What Should Pharmacists and Pharmacy Teams Advise?13
Pharmacists’ Role:
Counseling for Safe Use Even if certain sunscreens don’t meet their claims, pharmacists play a vital role in educating the public on how to use them correctly.
- Sun protection is essential every day. All skin types, including darker tones, require protection—even on cloudy days.
- Apply generously and reapply often. Use ~35 mL (about one teaspoon per body part: face/neck, each arm, leg, front, and back). Reapply every 2 hours and immediately after swimming, sweating, or toweling off.
- Match sunscreen type to patient needs.
- Lotions/creams: best for dry skin or full-body application
- Sticks: good for sensitive areas like lips or around eyes
- Sprays: convenient, but must be rubbed in evenly
- Zinc or physical blockers: ideal for sensitive or acne-prone skin
- Reinforce realistic expectations. Even high-SPF sunscreens allow some UV exposure. Encourage a multi-layered approach with shade, clothing, and sunglasses.
- Ensure pharmacy assistants are trained to confidently communicate these sun-safe strategies.
Conclusion
Know Your Skin. Protect Your Health.
Sunscreens remain a critical tool in the fight against melanoma, but must be used properly—and their quality must be held to the highest standard. In tandem with professional counseling and early detection, they form a vital frontline defense.