What is Endometriosis?1–3
Endometriosis is a chronic, inflammatory gynecological disorder where tissue resembling the endometrium—the lining of the uterus—grows outside the uterine cavity.The most widely accepted explanation for its origin is Sampson’s theory of retrograde menstruation, which suggests that menstrual blood flows backward through the fallopian tubes into the pelvic cavity, allowing endometrial cells to implant and grow. This misplaced tissue can be found on the ovaries, fallopian tubes, pelvic peritoneum, bladder, bowel, and in rare cases, even outside the pelvic region, such as the lungs or brain.
These ectopic endometrial implants respond to hormonal changes of the menstrual cycle just like the uterine lining does, bleeding and shedding. However, because the blood has no way to exit the body, it causes inflammation, scarring, adhesions, and debilitating pain.
At the molecular level, endometriosis is increasingly understood as a chronic inflammatory and immunometabolic condition. Elevated levels of pro-inflammatory cytokines such as interleukins (IL-6, IL-8) and tumor necrosis factor alpha (TNF-α) are consistently found in the peritoneal fluid of affected individuals. These cytokines recruit immune cells, perpetuate inflammation, and contribute to pain hypersensitivity and subfertility. In addition, recent findings highlight a dysregulation of adipokines, particularly low adiponectin levels, which may further exacerbate inflammation and hormonal imbalances within the peritoneal microenvironment, suggesting a novel metabolic-immune axis in the pathophysiology of endometriosis.
Adiponectin
Adiponectin is a cytokine produced predominantly by adipose tissue, playing significant roles in metabolism and homeostasis. It circulates in high concentrations (4–37 µg/mL), existing in different structural forms (trimer, hexamer, multimer), with the high-molecular-weight form being most biologically active. Physiological functions of adiponectin include:
Metabolic Regulation: It improves insulin sensitivity, lowers blood glucose, and promotes fat metabolism through AMPK activation.
Anti-inflammatory Actions: Reduces inflammation by modulating immune cells, such as promoting macrophages from inflammatory (M1) to anti-inflammatory (M2) phenotypes.
Anti-apoptotic and Anti-fibrotic Properties: Regulates cell death and tissue remodeling, potentially protecting organs from excessive fibrosis and cellular damage.
Angiogenesis Regulation: It generally inhibits pathological blood vessel growth, though its exact effect can vary depending on context.
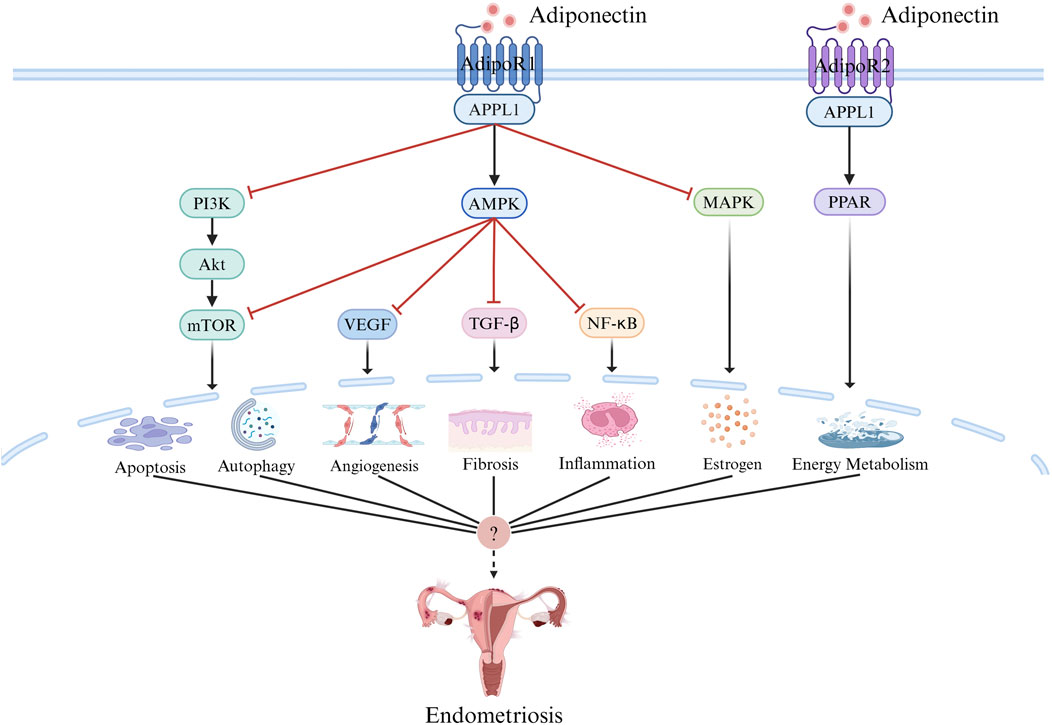
It acts mainly through three receptors:
- AdipoR1
- AdipoR2
- T-Cadherin
activating signaling pathways such as:
- AMPK
- PI3K/Akt/mTOR
- MAPK
- NF-kB
All implicated in the pathogenesis of endometriosis.
Endometriosis is not just a Bad Period—it is a complex disease.
Endometriosis is not just a “bad period”—it is a complex disease that can severely impact quality of life, mental health, sexual relationships, and fertility.
Who Gets It?4–6
Endometriosis affects approximately 10% of women of reproductive age globally—about 190 million people. In Australia alone, it’s estimated to affect 1 in 7 women. However, due to social stigma and diagnostic limitations, this figure may be underreported.
Risk factors include early menarche, short menstrual cycles, heavy bleeding, nulliparity (not having given birth), family history, and possibly environmental and genetic factors.
Interestingly, lifestyle habits such as prolonged breastfeeding, contraceptive use, and physical activity are thought to have a protective effect.
Despite its prevalence, many people with endometriosis go undiagnosed, particularly adolescents, marginalized populations, and those in low-resource settings
Symptoms7,8
The symptoms of endometriosis can vary widely, contributing to diagnostic delays that often exceed 6–10 years. Endometriosis is often described as the “Chameleon of gynecology” because of its elusive symptoms
“ Endometriosis is often described as the Chameleon of gynecology. ”
Common symptoms include:
- Chronic pelvic pain, especially before and during menstruation
- Painful periods (dysmenorrhea)
- Pain during or after sex (dyspareunia)
- Painful bowel movements or urination, particularly during periods
- Infertility
- Fatigue, bloating, nausea
- Depression and anxiety
In some cases, endometriosis can present with no symptoms at all. In others, it mimics conditions such as irritable bowel syndrome, interstitial cystitis, or even appendicitis, making diagnosis even more challenging.
Diagnosis9,10
Historically, definitive diagnosis required laparoscopic surgery with histological confirmation. However, this invasive method is no longer a prerequisite to initiate treatment. Initial diagnosis involves a thorough history and physical exam. Imaging tools like transvaginal ultrasound and MRI are increasingly used to detect ovarian endometriomas and deep infiltrating lesions. However, many cases remain undiagnosed due to symptom normalization and stigma surrounding menstruation.
Serological markers like CA-125 and newer candidates like miRNAs are under investigation but are not yet reliable for routine screening.
Treatment11–13
There is no known cure for endometriosis. Treatment is tailored to symptom severity, reproductive goals, and individual preferences, and may include: Pharmacological options:
- NSAIDs (e.g., ibuprofen, naproxen) for pain relief
Hormonal therapies such as:
Combined oral contraceptive pills (COCP)
Progestins (oral, depot, or IUDs)
GnRH analogues or antagonists (e.g., elagolix, relugolix)
Selective progesterone receptor modulators (SPRM)
Combined Oral Contraceptive Pills (COCP)
COCPs contain ethinylestradiol (an estrogen) and a progestogen (e.g. levonorgestrel). They help in endometriosis by:
- Suppressing ovulation and stabilizing hormonal levels.
- Reducing endometrial proliferation both in the uterus and at ectopic sites.
- Decreasing menstrual volume and frequency, thereby limiting retrograde menstruation.
- Inducing decidualization and atrophy of endometrial implants.
Regimens
| Regimen Type | Duration of Use | Bleeding Pattern | Best For |
|---|---|---|---|
| Cyclic | 21 days on, 7 days off | Monthly bleeding | Mild cases or personal preference |
| Extended | 9–12 weeks on, 4–7 days off | Quarterly bleeding | Moderate symptoms |
| Continuous | No breaks | Amenorrhea or spotting | Severe/recurrent endometriosis |
Choosing a Regimen: Decision is based on individual tolerance, symptom severity, and patient preference.
Typical COCP Formulations Used in Endometriosis
| Brand / Generic Name | Composition | Daily Dose |
|---|---|---|
| Microgynon 30® | Ethinylestradiol 30 mcg + Levonorgestrel 150 mcg | 1 tablet daily |
| Valette | Ethinylestradiol 30 mcg + Dienogest 2 mg | 1 tablet daily |
| Marvelon® | Ethinylestradiol 30 mcg + Desogestrel 150 mcg | 1 tablet daily |
| Yasmin® | Ethinylestradiol 30 mcg + Drospirenone 3 mg | 1 tablet daily |
| Yaz | Ethinylestradiol 20 mcg + Drospirenone 3 mg | 1 tablet daily |
| Qlaira® (Quadri-phasic) | Estradiol valerate 1–3 mg + Dienogest 2 mg (varies) | Follow specific pack instructions |
What is a “Quadriphasic” Pill?
Quadriphasic refers to a 4-phase dosing schedule in a single pill pack, mimicking natural hormone changes more closely than mono- or triphasic pills.
| Tablet Type | Contents | Days Taken |
|---|---|---|
| Phase 1 (light yellow) | Estradiol valerate 3 mg | Days 1–2 |
| Phase 2 (dark red) | Estradiol valerate 2 mg + Dienogest 2 mg | Days 3–7 |
| Phase 3 (light yellow) | Estradiol valerate 2 mg + Dienogest 3 mg | Days 8–24 |
| Phase 4 (pink) | Estradiol valerate 1 mg | Days 25–26 |
| Placebo (white) | No active ingredients | Days 27–28 |
Progestins (Oral, Depot, or IUD)
Oral Progestins
| Brand | Drug | Dose Frequency | Duration |
|---|---|---|---|
| Primolut N | Norethisterone | 5 mg 2–3 times daily | Long-term use with review every 6–12 months |
| Visanne | Dienogest | 2 mg once daily | Approved for long-term use (≥15 months) |
| Slinda | Drospirenone | 4 mg daily (24 active + 4 placebo) | Daily use |
Depot Progestins
| Brand | Drug | Administration | Duration |
|---|---|---|---|
| Depo-Provera | Medroxyprogesterone acetate | 150 mg IM every 12 weeks | Review after 2 years (bone health) |
| Noristerat | Norethisterone enanthate | 200 mg IM every 8 weeks | Short-term (~6 months); periodic review |
Intrauterine Devices (IUDs)
| Brand | Drug | Daily Release | Duration |
|---|---|---|---|
| Mirena | Levonorgestrel 52 mg | ~20 mcg/day | Up to 5 years (8 years for contraception) |
| Kyleena | Levonorgestrel 19.5 mg | ~17.5 mcg/day | Up to 5 years (off-label for endometriosis) |
GnRH Analogues or Antagonists
GnRH Agonists
Initially stimulate, then downregulate GnRH receptors, causing estrogen suppression (pseudo-menopause).
| Drug | Brand | Route | Dose | Duration |
|---|---|---|---|---|
| Leuprorelin | Lucrin Depot | IM | 3.75 mg/month or 11.25 mg/3-monthly | 6–12 months (with add-back) |
| Goserelin | Zoladex | SC implant | 3.6 mg every 28 days | Max 6 months (longer with add-back) |
| Nafarelin | Synarel | Intranasal | 200 mcg twice daily | 6 months |
Add-back therapy (e.g. norethisterone or tibolone) is recommended beyond 6 months to mitigate menopausal side effects and bone loss.
GnRH Antagonists
Directly block GnRH receptors, suppressing LH/FSH without flare-up.
| Drug | Route | Dose | Duration |
|---|---|---|---|
| Elagolix | Oral | 150 mg once or 200 mg twice daily | 6–12 months |
| Relugolix | Oral | 40 mg daily | Emerging in AUS |
| Relugolix combo | Oral | Relugolix 40 mg + Estradiol 1 mg + Norethisterone acetate 0.5 mg | Approved overseas |
| Linzagolix | Oral | — | Under clinical trials |
Selective Progesterone Receptor Modulators (SPRMs)
Ulipristal acetate is a partial progesterone antagonist.
- EllaOne: 30 mg single dose – emergency contraception
- Esmya: 5 mg daily for 3 months – for fibroids
- Not yet approved for endometriosis
Agents explored in trials for endometriosis include:
- Ulipristal
- Asoprisnil
- Telapristone
- Vilaprisan
Note: None are yet approved for endometriosis treatment.
Surgical options:
- Laparoscopic removal of lesions, adhesions, and endometriomas
- Excision of deep infiltrating endometriosis
Surgery is often considered when medical therapy fails or in cases of infertility. However, recurrence is common—affecting up to 67% of cases within five years post-surgery.
Complementary treatments such as physiotherapy, psychological counseling, and dietary modifications can support holistic care.
The Role of the Pharmacist14,15
Pharmacists are uniquely positioned as accessible healthcare professionals who can play a transformative role in the early detection and management of endometriosis.
Symptom Recognition and Timely Referral
Pharmacists are often the first point of contact for individuals experiencing menstrual pain, gastrointestinal discomfort, or fatigue. By recognizing red flags—such as chronic pelvic pain unresponsive to first-line analgesics, dyspareunia, or cyclical bowel symptoms—pharmacists can prompt timely medical referrals, significantly reducing diagnostic delays.
Education and Destigmatization
Menstrual pain is often normalized in society. Pharmacists can help break this stigma by validating patients’ experiences and creating a safe environment to discuss symptoms.
Avoiding dismissive language such as:
“It’s just period pain”
“You don’t look sick”
“Are you sure it’s not just stress?”
‘Everyone goes through this’:
Instead, pharmacists might ask:
“Do you experience pain during intercourse or bowel movements around your period?
“Have your symptoms affected your ability to work or attend school?”
“Would you consider tracking your symptoms to identify any patterns?”
Pharmacological Counselling
As medication experts, pharmacists can ensure safe and effective use of hormonal treatments and analgesics. They counsel patients on potential side effects, monitor adherence, and provide guidance on the risks of long-term NSAID or opioid use. Emerging therapies such as GnRH antagonists or Selective Progesterone Receptor Modulators (SPRM) require pharmacist involvement to monitor adverse effects such as hypoestrogenism and bone density loss.
Supporting Self-Management and Quality of Life
Pharmacists can empower patients through:
- Tailored advice on lifestyle modifications
- Referrals to support groups or specialist care
- Tracking treatment response and side effects
- Coordinating care across multidisciplinary teams
Pharmacists also play a role in encouraging ongoing therapy and providing reassurance during relapses or medication transitions.
Conclusion
Endometriosis is a chronic, misunderstood, and underdiagnosed condition that affects millions globally. While no cure currently exists, effective symptom control and improved quality of life are achievable through timely diagnosis, evidence-based treatment, and holistic support. Pharmacists, as trusted and accessible healthcare providers, are ideally positioned to champion early recognition, reduce stigma, and support the multidisciplinary management of endometriosis. With continued investment in education, research, and public health initiatives, we can shift the paradigm from normalization of suffering to proactive care and empowerment.